The decision of how to treat medical conditions can be overwhelming. Many patients research all potential options. Others follow their doctor’s advice. Some just go with standard procedures. Regardless of how you approach this decision, accurate information is crucial.
Regenexx is a world-wide network of select, highly skilled physicians specially trained in regenerative procedures established by Chris Centeno, MD. Regenexx has developed a regulated system that provides standardized processing kits and procedure consistency so that efficacy rates can be credibly established. All Regenexx patients participate in a world-wide registry to add to this database The live registry allows patients to review for themselves the success rate of procedures to provide accurate information while deciding on a treatment approach. Dr. Centeno constantly reviews information and misinformation published about regenerative procedures, debunking publications containing research deemed inadequate. In the below meta-analysis, several factors were common in studies that showed failed efficacy for PRP: 1) insufficient concentration from inferior PRP kits 2) treatment dose.
2023 Meta-analysis of Randomized Clinical Trials of PRP
A 2023 meta-analysis by Chris Centeno, MD, examined the published literature on interventional orthobiologics, specifically on PRP for all musculoskeletal indications. C. Centeno. 2023 PRP RCT Infographic and Study Failure Analysis; July 29, 2023. Not only has the number of randomized controlled trials (RCTs) on PRP significantly increase recently, but he found that there is more and better literature support for the use of PRP in many orthopedic indications than exists for orthopedic surgery as a field. C. Centeno. The Evidence Supporting Common Orthopedic Surgeries Is AWFUL; July 22, 2021. In previous research, Dr. Centeno found a few studies in which PRP failed to show superiority versus placebo. In his 2023 meta-analysis, Dr. Centeno also examined why some studies showed PRP failure as a treatment. Below is an infographic that depicts his findings for 107 RCTs. For a clearer depiction, please see the original article on study failure mentioned above.
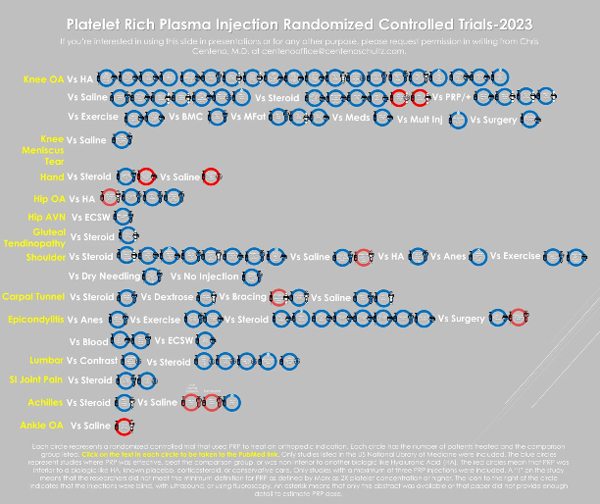
Each circle represents a randomized controlled trial that used PRP to treat an orthopedic indication. Each circle has the number of patients treated and the comparison group listed. Click on the text in each circle to be taken to the PubMed link. Only studies listed in the US National Library of Medicine were included. The blue circles represent studies where PRP was effective, beat the comparison group, or was non-inferior to another biologic like Hyaluronic Acid (HA). The red circles mean that PRP was inferior to a biologic like HA, known placebo, corticosteroid, or conservative care. Only studies with a maximum of 3 PRP injections were included.
- A white asterisk (*) on the study circle = the full text was not available or the paper never discussed how investigators made the PRP.
- The syringe icons
 = how the injection was done.
= how the injection was done. - The blindfold icon
 = the injection was blind
= the injection was blind - The ultrasound probe
 = the injection was guided using ultrasound.
= the injection was guided using ultrasound. - The radiation icon
 = fluoroscopy guided.
= fluoroscopy guided. - A white exclamation point
 on the circle indicates the study didn’t meet the 2 times (2x) platelet concentration standard.
on the circle indicates the study didn’t meet the 2 times (2x) platelet concentration standard.
From C. Centeno. 2023 PRP RCT Infographic and Study Failure Analysis; July 29, 2023.
RCT analysis that showed failed efficacy of PRP injection vs placebo
Study failure was defined as PRP being less effective than hyaluronic acid, or steroid injection, or saline. In this meta-analysis, 11 studies (10%) met the definition of failed. The red circles in the infographic represent outcome failures. However 90% of studies (blue circles) showed successful treatment with PRP.
Insufficient Concentration
Dr. Centeno states that some of the failed studies did not use a PRP concentration as defined by acceptable standards of at least 2x a greater concentration of platelets than typically found in whole blood. He observed that this is a particular problem for older patients who need high platelet concentration (Berger et al. Bone Joint Res. 2019 Feb 2;8(1):32-40). For example, two of the most commonly used PRP kits (Kits A & B for the purposes of this blog) can deliver the minimum 2x concentration required if the efficiency of platelet isolation is 100%. However, this is not the case with either Kit A or Kit B. Both typically draw 8-10 mL of whole blood that produces about 3-4 mL of PRP product for injection. But, based on independent lab data, Kits A & B proved 48% (1.3x) and 46% (1.6x) efficient, respectively, neither achieving the 2x concentration standard for "real PRP." The studies in the meta-analysis that used these kits are labeled as non-PRP based on existing data and are flagged with an exclamation point.
Platelet Dose
A less common factor that affects the efficacy of PRP treatment is dose. Dr. Centeno cites one published study of a 5x concentration using a double spin technique, but the total platelet concentration dose was only 1 mL. The infograph shows that 60% of the total outcome failures used PRP product that was below the platelet threshold needed (fake PRP); 5% of studies that used real PRP also had outcome failure. Notably, about 15% (15/101) of studies using a below-platelet-threshold PRP product showed success. Several factors may account for study failures using real PRP:
- Injection blinding and imaging guidance. It has been reported that blind injections are associated with worse outcomes. In addition, performing a knee intra-articular injection without image guidance, for example, can miss the joint 20%-25% of the time. Technique- and operator-dependence likely affected efficacy.
- Cell-toxic anesthetics. Other substances that are injected, such as cell-toxic anesthetics (eg, bupivaccine, lidocaine), are associated with treatment failure.
- Corticosteroid injections. Prior steroid injections in a specific area are associated with higher surgical failure rates, because they reduce the ability to heal.
Source of studies found on original article.
Why this matters
Dr. Minotti has written frequently about the need for regulation in the field of regenerative medicine so that subpar procedures and providers can be weeded out from legitimate clinics. To this end, physicians themselves have formed networks to help establish standards that allow for credible research input and valid outcomes. This is the first of a series to help patients accurately assess both good and bad information published on Regenerative Orthopedics.
Christopher J. Centeno, MD, is an international expert and specialist in Interventional Orthopedics and the clinical use of bone marrow concentrate in orthopedics. He is board-certified in physical medicine and rehabilitation with a subspecialty of pain medicine through The American Board of Physical Medicine and Rehabilitation. Dr. Centeno has chaired multiple international research-based conferences. He also maintains an active research-based practice, with multiple publications listed in the US National Library of Medicine.

