Platelet Rich Plasma (PRP)
Platelet Rich Plasma Therapy (PRP), an innovative and increasingly popular cellular treatment in Regenerative Orthopedics, promotes and accelerates the body's natural healing process for soft tissue injuries and osteoarthritis. PRP uses your own blood cells in concentrated doses to stimulate the natural healing process for musculoskeletal injuries and reduce joint inflammation to help reverse the degenerative effects of osteoarthritis.
How Does PRP Therapy Work?
Blood contains amazing healing power with many types of cells working to maintain the health of the entire body. Platelets were once thought to only function in formation of blood clots. They are one of the first cells to rush to an injury to stop bleeding. Research has since discovered that platelets also contain growth factors, such as alpha-granules, and tissue building proteins that are central to tissue repair. Platelets stimulate release of localized stem cells through a process called "signaling." Mesenchymal stem cells then direct the complex procedure of cellular healing.
Read more about how our body creates new tissue.
If our bodies heal themselves, why is PRP sometimes needed?
- PRP condenses platelet cells to magnify their healing capacity, accelerating and enhancing the healing process.
- Plasma, the liquid portion of blood, acts primarily as a transport medium for blood cells, nutrients, and metabolic waste products.
- Collagenous tissue, such as tendons, ligaments and cartilage, have extremely poor blood supply, causing these tissues to heal slowly and often incompletely.
- Platelets stimulate activation of localized stem cells and promote a healing response in surrounding tissue.
Regenexx is a world-wide network of select, highly skilled physicians who are specially trained in interventional procedures for orthopedic conditions. Regenexx provides the world's most advanced, research-driven, regenerative orthopedic procedures in North America, Europe, the Middle East, Asia and Australia. Specializing in advanced non-surgical procedures for joint Injuries, osteoarthritis, and other orthopedic conditions, Dr. Minotti brings these procedures to you!
If you have injured your knee or if normal wear and tear has caused degeneration of your joint, stem cell therapy may help. It uses your own bone marrow to help repair knee damage. It may help you avoid surgery.
To determine if Regenerative Orthopedics will be helpful for you, please tell us about your condition.
Leader in Orthobiologic Treatment for Musculoskeletal Conditions

Dr. Minotti began performing Orthobiologic Therapy in 2007 and has treated hundreds of patients with amazing success. 86% of his patients have found significant relief from pain and restoration of musculoskeletal function.
Dr. Minotti is specialty trained in Neuromusculoskeletal Medicine. He combines his intensive training in the musculoskeletal system with advanced training in Regenerative Medicine, specifically as applied to orthopedic conditions. He conferences regularly with the world’s leading physicians to provide his patients with the most effective treatments that science has to offer.
Founder of North Texas Musculoskeletal Medicine in Southlake TX, Dr. Minotti believes that orthobiologic procedures, such as Platelet Rich Plasma (PRP) and Stem Cell Therapy, are a new frontier in medicine, offering treatments that effectively bridge the gap between medications that mask pain and invasive surgery. He has helped thousands of patients find freedom from pain to restore their quality of life. Dr. Minotti is honored to be recognized by his peers with the Top Docs award. He also serves as an adjunct professor at University of North Texas Health Science Center.
Common Applications
Numerous conditions can be considered for PRP. Based on current research and clinical experience, moderate to severe cases of osteoarthritis and tendon injuries show promising results.
• Knee Pain – Osteoarthritis, Meniscus Tears, Chondromalacia Patella, Tendon Injuries, Ligament sprains or tears.
• Hip Pain – Osteoarthritis, Hip Labrum Tears, SI Joint Arthritis, Gluteal tendon tears, Iliotibial Band (ITB) Syndrome
• Shoulder – Osteoarthritis, Rotator Cuff Tendinitis, Tendinopathy, or Tears, Labrum Tear, Bicipital Tendinitis
• Elbow Pain – Lateral Epicondylitis (Tennis Elbow), Medial Epicondylitis (Golfers Elbow), Osteoarthritis
• Wrist/Hand Pain – Osteoarthritis, DeQuervain’s Tenosynovitis
• Ankle & Foot Pain – Achilles Tendinitis or Partial Tears, Plantar Fasciitis Ankle sprains/ligament injury
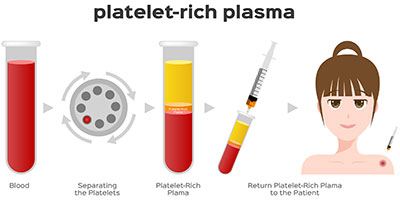 PRP: Procedure Snapshot
PRP: Procedure Snapshot
The patient's blood is drawn and spun in a centrifuge to isolate the platelets and their associated growth factors. This process increases the level of platelets from a concentration of 6% to 94%. Concentrated platelets are added to the patient's plasma. Plasma contains a variety of proteins that are essential to connective tissue healing. Using ultrasound guidance, this preparation is then injected into the damaged area, stimulating release of stem cells that accelerate and enhance new cell growth. Collagen molecules are subsequently deposited on the damaged tissue, resulting in tissue regeneration and restored blood flow.
Because the injected solution is prepared from the your own blood using aseptic technique, your body has no risk of rejection or exposure to blood-borne diseases.
The procedure takes about 1 hour and the patient can return home the same day. Healing from the procedure takes about 1 week. Healing of injured tissue depends on the severity of the injury and healing tendencies of the individual. Many patients feel pain relief within weeks of the procedure. Follow up injections 6 months later can boost the initial treatment for increased healing and pain relief.
Adverse reactions associated with PRP injections are remote and usually of minor severity-most commonly, injection site pain and infection.
Scientific advances in the understanding of how the body actually heals through tissue regeneration, combined with rapid developments in stem cell biology, have truly created a renaissance in medical treatment. Stem cells, like other medical products that are intended to treat, cure or prevent disease, require U.S. Food and Drug Administration (FDA) approval before they can be marketed. At this time, only cells harvested from the patient’s own body and that are only minimally manipulated have been approved by the FDA.
Additionally, devices that allow physicians to minimally manipulate blood, bone marrow and adipose tissue for the treatment of orthopedic conditions also require FDA approval. NTXMSK recognizes and welcomes the FDA’s important role in assuring patient safety. All of our treatment protocols are compliant with the published FDA guidelines regarding the use of human cells, tissues, and cellular or tissue-based products.
We Can Help
To learn more about what we can do to help with your condition, call our office at 817-416-0970. We will thoroughly diagnose your condition and present you with treatment options. From there we will guide you along your road to recovery.

