Renaissance means rebirth or regeneration. Every few generations medicine takes a major turn. We’re at one of those junctures now with regenerative medicine — where healing is triggered from within the human body. It’s bringing a whole new universe to how physicians provide care. Deer grow, shed and then regrow their antlers. Sea stars sacrifice but then regrow their arms. This is regeneration, and every species — from amoeba to human — is inherently capable of it to some degree… -Mayo Clinic Center for Regenerative Medicine
Musculoskeletal Healing: Why sometimes injuries heal and why sometimes they don’t
The ability to heal is determined by many factors, some known and some unknown. We do know that when healing is incomplete, tissue damage becomes chronic, leading to arthritis, mechanical dysfunction and harmful stress to adjoining structural areas. Healing of musculoskeletal injury requires that our bodies are able to supply the necessary healing units, much like an Emergency Response Team, with each unit doing its job in turn. “Dynamic Equilibrium” exists when cell degeneration is in equal ratio to cells available for regeneration. Injury, arthritis and poor cellular health disrupt this homeostasis. Adequate cells for repair are unable to keep pace with healing requirements.
Chronic injury generally results in uncontrolled inflammation as our body struggles to supply healing nutrients and growth factors. Our body senses injury and responds as it does with any injury: through cell signaling, rushing the necessary cells to the site. This process is miraculous and keeps our bodies healthy. When the injury does not heal completely, the process known as inflammation becomes uncontrolled, causing further damage to tissue and arthritis. Localized stem cells, critical in the process, become depleted.
Click here to learn how to address the root cause of your joint pain with Orthobiological Treatments
Joint injury
Tissue damage to joints is particularly difficult to heal due to their complex structure and the nature of soft tissue encapsulating the joint. Movement happens not only by the muscles that move our skeletal system, but also through coordination of collagenous tissues surrounding the joints:
- Ligaments that hold the bones together
- Tendons that attach the muscles to the bones
- Articular cartilage that lubricates and acts as a shock absorber between the bones.
Muscle tissue has a healthy flow of blood that adequately supplies nutrients, growth factors, and oxygen, while removing metabolic waste to prepare the site for healing. This is apparent in the red color of muscles. Ligaments, tendons and cartilage, however, are white in color, as the blood supply to these tissues is poor. The oxygen consumption of tendons and ligaments is 7.5 times lower than that of skeletal muscles. The low metabolic rate and well-developed anaerobic energy generation capacity are essential to carry loads and maintain tension for long periods. However, a low metabolic rate results in slow healing after injury. When acute or chronic injury occurs in these tissues, healing is slow and often incomplete.
Blood flow is crucial in the healing process. The liquid portion of blood, plasma, acts as a transport medium for blood cells, nutrients, and removal of metabolic waste products to prepare the site for healing. Platelets, once thought to merely help with blood clotting, contain growth factors called alpha granules and help to stimulate the release of localized stem cells. When the amount of localized stem cells and necessary nutrients required for healing become depleted or the body is able to supply only limited blood flow, healing sometimes needs a little help. Learn more about tendon injury.
 Tendon and ligament injury account for about half of all musculoskeletal injuries.
Tendon and ligament injury account for about half of all musculoskeletal injuries.
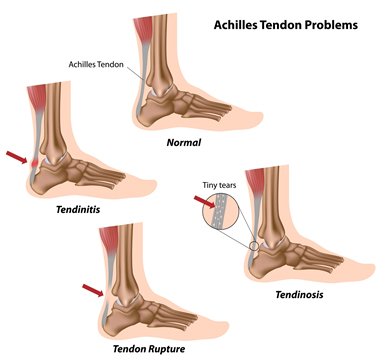
Injury to a tendon, for example, can occur when repeated use of a muscle causes stress on the tendon that attaches it to the bone. This repeated stress can result in micro-tears, a form of tendinopathy called tendinosis, or a “strain.” A common example of this is Golfer’s Elbow or Tennis Elbow. Because of poor blood supply to this thick cartilaginous tissue, strains are slow to heal. When left untreated, the weakened tissue can rupture, which is often the situation with a torn rotator cuff, slap tear, or ruptured Achilles tendon, conditions that heal slowly and rarely completely.
Damaged ligaments become stretched or lax, causing bones in the joint to shift. This movement causes pain, muscle spasms, and eventually arthritis. When stretched, small nerve fibers in damaged ligaments transmit pain impulses to the brain. Through a subconscious reflex, the surrounding muscles go into a painful spasm in an attempt to stabilize the joint. Often, painful knots appear in the surrounding muscles. Muscles become tight and painful as they try to compensate for the weak and damaged underlying structures. Spasm in the muscles further decreases the blood flow and delivery of nutrients to the tissue, contributing to continued tissue breakdown. The chronic tension from the muscles in spasm leads to deterioration of the tendon attachments, resulting in tendinosis, chronic tendon degeneration.
Slow healing promotes formation of scar tissue that inhibits smooth musculoskeletal function. During healthy repair, cells regenerate with necrotic cells being replaced by new ones, the body’s natural process of regeneration. When healing is inhibited due to poor blood supply and lack of necessary growth factors, nutrients and proteins, slow, incomplete healing occurs. Rather than healthy regeneration of cells, injured tissue is partially replaced by scar tissue that restricts the natural function of the musculoskeletal system.
Physiology of Intrinsic healing
Ligaments, tendons and cartilage contain similar biological structure. Healing of these tissues is divided into four overlapping stages with the body functioning similarly to an emergency response team with each biological function doing its own job in turn. Some conditions will always require surgery, particularly when none of the damaged tissue is intact. Orthobiologic procedures provide condensed amounts of natural healing factors to accelerate and enhance healing for a majority of musculoskeletal conditions.
The Four Stages of Musculoskeletal Healing
- Post injury First 72 hours
The body's first response is to protect itself. Blood containing platelet cells rushes to the area to stop bleeding and initiate the healing process.
Platelets are the most numerous cells shortly after a wound occurs, releasing cytokines, small proteins important in cell signaling, and growth factors. Growth factors stimulate cells to speed their rate of division. Platelets, also, release other chemicals that stimulate the inflammatory phase.
- Inflammatory First week
Inflammation is the body's natural response to defend against harmful substances. As the blood vessel become dilated, swelling quickly occurs.
A special category of white blood cells that originate in the bone marrow rush to the area as first responders. Two types of leukocyte are predominant in the inflammatory response- macrophages and neutrophils. Neutrophils are first to the injured site and function by neutralizing harmful bacteria. Macrophages aid the healing process by engulfing bacteria and dead cells, ingesting them so that the area is clear for new cells to grow.
- Proliferation weeks 3-6
Swelling and pain begin to subside and proliferation of cells begins to repair the injury.
Proliferation is when the body begins to produce new cells and tissue. Special cells called Fibroblasts create a framework of collagen for new cells to develop, essentially sewing the two bits of damaged tissue back together. Collagen is the universal building material for most tissue in the body.
In soft tissue, collagen is organized in straight lines, allowing the stress to dissipate evenly through the tissue when it is stretched. However, Collagen formed during the Proliferation Stage is constructed in a random fashion. This happens because the body is trying to repair the area quickly. As a result, the repair site is left weak and susceptible to further injury.
- Maturation Week 6-18 months
New blood vessels mature and the tissue now becomes stronger with more organized and healthy fibers. Pain subsides. Collagen density and tissue strength are increased.
Scar tissue, part of the proliferation phase, generally causes adhesion formation that inhibits mechanical function.
When healing is enhanced through cellular regenerative procedures, repair provides increased collagen deposit resulting in reduced scar tissue.
Intrinsic healing through an accelerated process results in better biomechanics, particularly a better gliding motion in the tendon sheathe.
Treatment for joint injury
The use of orthobiologics in treatment of musculoskeletal conditions is an emerging field with evidence of its success accelerating rapidly. Research examining the complex biological mechanisms of cellular health and tissue regeneration is extensive, particularly the behavior of platelets, stem cells, immune system cells and natural growth factors in the blood. The clinical application of Regenerative Orthopedics has demonstrated promising results and a high safety profile. Learn more.
Pain in musculoskeletal injury is often caused by inflammation, a sign that the body is trying to heal. Controlled levels of inflammation are necessary for healing. Anti-inflammatory drugs and cortisone injections are effective at reducing pain and inflammation, but do not have a healing effect. Actually, they have an inverse effect on healing. By inhibiting the body’s natural EMR unit that responds by rushing blood and healing factors to the site of injury, cortisone and a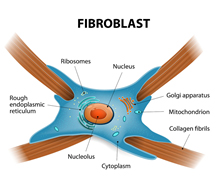 nti-inflammatory medications ultimately block the body’s production of collagen, the primary component of tendons, ligaments and other cartilaginous tissue. By masking the injury, anti-inflammatory drugs can also lead to complete rupture.
nti-inflammatory medications ultimately block the body’s production of collagen, the primary component of tendons, ligaments and other cartilaginous tissue. By masking the injury, anti-inflammatory drugs can also lead to complete rupture.
Regenerative orthobiologic procedures have been used to treat pain and injuries for more than sixty years with consistent and positive results. With advancement in technology and science, PRP and Stem Cell Injections are changing the way physicians treat orthopedic conditions. Through stimulation of the body’s natural healing response, the root cause of pain or dysfunction are addressed rather than merely masked by medication. Regenerative orthobiologic procedures supply the needed help that your body sometimes needs. Suffering with pain from chronic musculoskeletal injury or arthritis is no longer necessary.
Leader in Orthobiologics
 Dr. Minotti is certified in Neuromusculoskeletal Medicine by the American Board of Neuromusculoskeletal Medicine with advanced training in Regenerative Medicine. His primary focus is Regenerative Orthopedics, nonsurgical, orthobiologic procedures designed to accelerate regeneration of cells in healing of acute and chronic musculoskeletal injuries.
Dr. Minotti is certified in Neuromusculoskeletal Medicine by the American Board of Neuromusculoskeletal Medicine with advanced training in Regenerative Medicine. His primary focus is Regenerative Orthopedics, nonsurgical, orthobiologic procedures designed to accelerate regeneration of cells in healing of acute and chronic musculoskeletal injuries.
Founder of North Texas Musculoskeletal Medicine in Southlake TX, Dr. Minotti is a pioneer in the field of regenerative medicine. He believes that orthobiologic procedures such as PRP and Stem Cell Therapy are a new frontier in medicine, offering treatments that effectively bridge the gap between medications that mask pain and invasive surgery. As scientists learn more about the physiology of how our bodies heal, healthcare is able to use this research to find new and better treatments.
Dr. Minotti is honored to be recognized by his peers with the Top Docs award for the fourth consecutive year. He also serves as an adjunct professor at University of North Texas Health Science Center.

