
I am Dr. Minotti, a regenerative medicine specialist. I have spent the past 18 years exploring new and better ways to treat the human body. I help frustrated patients find freedom from pain and restore their quality of life so they can do the things they love.
Research exploring the physiology of how the body actually heals has allowed innovative advancements in treatment of musculoskeletal conditions. Regenerative Orthopedics helps bodies mend themselves, providing real results for people who have been living ‐ until now ‐ with few treatment options. Regenerative Orthopedics effectively bridges the gap between invasive surgery and medications that mask pain.
Getting older is inevitable… old and creaky is not! So, how do we keep our bodies working at their best? How do we maintain the quality of life we desire? What are our treatment options?
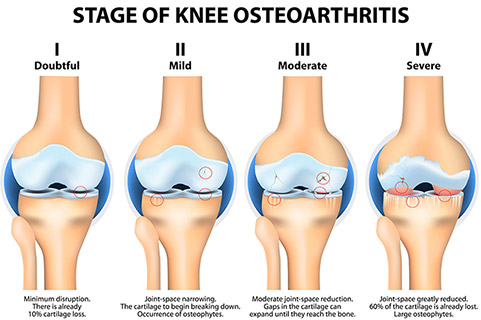
Osteoarthritis, also called degenerative arthritis, is the most common type of this crippling disease. Aging is a prime factor in osteoarthritis—life can cause wear and tear on our joints. However, chronic and partially healed joint injuries also play a major role in the advancement of arthritis. Genetics and lifestyle can also be factors. Both men and women have the disease, but it’s more common in people who are overweight and in those with jobs that stress particular joints.
As the smooth articular cartilage between the joints wears down, rubbing together of the bones causes friction and inflammation. Bone spurs often develop at the side of the joints and the bone underneath the cartilage hardens. These changes cause pain, swelling and problems moving the joint. Because of pain and decreased physical activity, the muscles that support the joints can weaken, creating further stress on the joint.
As chronic injury and arthritis persist, localized, somatic stem cells are no longer able to keep pace with the increasing demand for tissue regeneration. When a reverse reaction occurs, as in cell degeneration with arthritis, balance must exist in equal ratio to reactants, or cells available for regeneration. This balance is referred to as “Dynamic Equilibrium.” Injury, arthritis and poor cellular health disrupt this homeostasis as adequate cells for repair are unable to keep pace with healing requirements. When this imbalance occurs, your body needs a little help.
Traditional treatment for arthritis has focused on treating the inflammation and pain associated with this condition. Although pain relievers can make you feel better, they do not change the course of the disease and can actually make it worse. Cortisone will reduce inflammation, but in turn inhibit healing and further damage cartilage.
Traditional Arthritis Treatments: Medications, Steroids, and Surgery
Surgery: Research on Unrelieved Chronic Pain
Most patients believe there is a 90% chance they will be pain free after joint replacement. However, 44% of knee-replacement patients have pain (15% severe to extreme persistent pain) three to four years after surgery.
Metsna, V., S. et al. Medicina (Kaunas) 50, issue 2, (2014): 82–6. doi: 10.1016/j.medici.2014.06.001.
Up to 54% have pain five years after knee replacement, showing an increase in patients with pain from year to year. Of the 54% with knee pain at five years, 87% of those develop knee pain only after surgery; 27% of hip-replacement patients still have pain three to four years after surgery.
Wylde, V., S. et al. Pain 152, issue 3, (March 2011): 566–72. doi:10.1016/j.pain.2010.11.023.
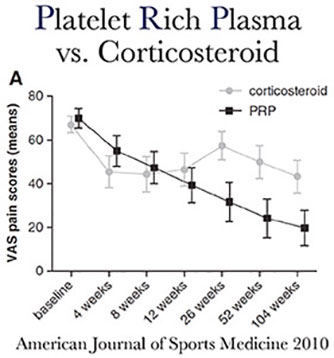
Steroids, Commonly Known as Cortisone
Cortisone temporarily stops the pain of injured joints by reducing inflammation. However, the body heals by Inflammation. When a person sprains an ankle, the persistent swelling for one to three days is the body’s attempt to heal the area. The healing cascade resulting from a rush of cells to the damaged area is inhibited by cortisone as it minimizes the migration of the immune cells to the injured area. Cortisone, along with epidural steroid injections, will reduce inflammation, but in turn inhibit healing and further damage cartilage. Healing is sacrificed healing for pain control.
Medications
To date, pain medications have been a primary solution for painful arthritis. However, pain medications do not address the root cause of your pain and actually have an inverse effect on the healing process by reducing inflammation. Inflammation is your body's natural healing response to tissue damage. Raging, chronic inflammation common with arthritis must be controlled, but elimination of this process stops the healing process.
Regenerative Orthopedics: Non-surgical Treatments for Arthritis

Platelet Rich Plasma
Blood contains amazing healing power with many types of cells working to maintain the health of the entire body. Plasma, the liquid portion of blood, acts primarily as a transport medium for blood cells, nutrients, and metabolic waste products, contributing to the physiological stability of the body. Plasma is mostly water, but contains proteins that reduce pain and inflammation. Blood cells called macrophages remove damaged tissue to clean the injured area in preparation for the healing process.
Another cell in the blood, platelets, were once thought to only function in formation of blood clots. Research has since discovered that platelets also contain growth factors, such as alpha-granules, and tissue building proteins that are central to tissue repair. Platelets stimulate release of localized stem cells through a process called "signaling." By harvesting and condensing platelet cells, their healing capacity is magnified and then injected back into the body, targeting damaged tissue to accelerate and enhance the healing process. PRP injections utilize platelets to stimulate activation of somatic, or localized, stem cells to promote a healing response in surrounding tissue.
Bone Marrow Aspirate Concentrate, Commonly Known as Stem Cell Therapy
Stem Cells are present in all of us, acting like a repair system for the body. They are sometimes referred to as “master cells” in that they have the potential to become many different specialized cell types. They act as an unlimited supply of repair cells, continually dividing throughout our lifetime. With increased age or chronic injury, the optimal amount of stem cells is often not delivered to an injured area. The purpose of Stem Cell Therapy is to amplify the natural repair system to keep pace with these demands to maintain healthy function of the musculoskeletal system.
Bone Marrow Stem Cell Therapy (BMAC) harvests healing cells from your own bone marrow to inject back into your body at the site of damaged tissue. Stem cells contained in the bone marrow are pluripotent, meaning they can divide into many types of cells. More importantly, growth factors and nutrients contained in the marrow aid in the formation of new blood vessels, activation of endogenous stem cells, modulation of the immune system, and growth of new cells and tissue. BMAC is a method of medical treatment using your own natural healing properties to help you find a better quality of life.
Currently, FDA approved bone-marrow derived MSCs are an excellent option for treatment of acute and chronic musculoskeletal conditions.
Read more about current FDA regulations
Research on Stem Cell Therapy and Arthritis: What Science is Telling Us
Articular cartilage has a limited capacity to repair following injury. Early intervention is required to prevent progression of focal traumatic chondral and osteochondral defects to advanced cartilage degeneration and osteoarthritis... Transplantation of mesenchymal stem cells (MSCs) is a promising strategy given the high proliferative capacity of MSCs and their potential to differentiate into cartilage-producing cells - chondrocytes.
Troy D Bornes, et al. Arthritis Research & Therapy201416:432
Among the various forms of degenerative joint disease, osteoarthritis (OA) is by far the most common and represents a painful chronic condition that can affect any synovial joint... Mesenchymal stem cells (MSCs) have been proposed as an optimal regenerative cellular therapeutic for degenerative musculoskeletal conditions like OA. These cells are found in a variety of tissues and have the ability to rapidly proliferate and differentiate to musculoskeletal lineages including bone and cartilage. A significant body of research has also demonstrated that these cells orchestrate important immunologic functions through modulation of the local inflammatory response. Taken together, these factors support the theoretical ability of MSCs to deter degenerative joint disease.Leader in Regenerative Orthopedics

Dr. Minotti is specialty trained in Neuromusculoskeletal Medicine and certified by the American Board of Neuromusculoskeletal Medicine. With advanced training in Regenerative Medicine, Dr. Minotti's primary focus is Regenerative Orthopedics, nonsurgical procedures designed to accelerate regeneration of cells in healing of acute and chronic musculoskeletal conditions. Dr. Minotti is highly regarded within the medical community, particularly sought after as a specialist in addressing knee pain, back pain, and shoulder pain conditions.
Dr. Minotti has devoted his professional career to being at the forefront of Regenerative Orthopedics and musculoskeletal care. With over 20 years experience as a Neuromusculoskeletal Specialist, he provides patients with a tailored approach to managing joint pain, injuries, and osteoarthritis.
The use of Regenerative Medicine in treatment of musculoskeletal conditions is an emerging field with evidence of its success accelerating rapidly. Research examining the biological mechanisms of cellular health and tissue regeneration is extensive, particularly the behavior of platelets, stem cells, and natural growth factors in the blood. Who is actually performing your procedure matters! Learn more about Dr. Minotti.

